In medical billing, one of the most common questions coders and providers face is whether CPT 99496 (Transitional Care Management) and CPT 99214 (Established Patient Office Visit) can be billed together. The answer depends on specific documentation, timing, and payer rules, especially Medicare. Let’s explore how these two codes interact, when they can and cannot be billed together, and how to ensure compliance while maximizing reimbursement.
Understanding CPT 99496
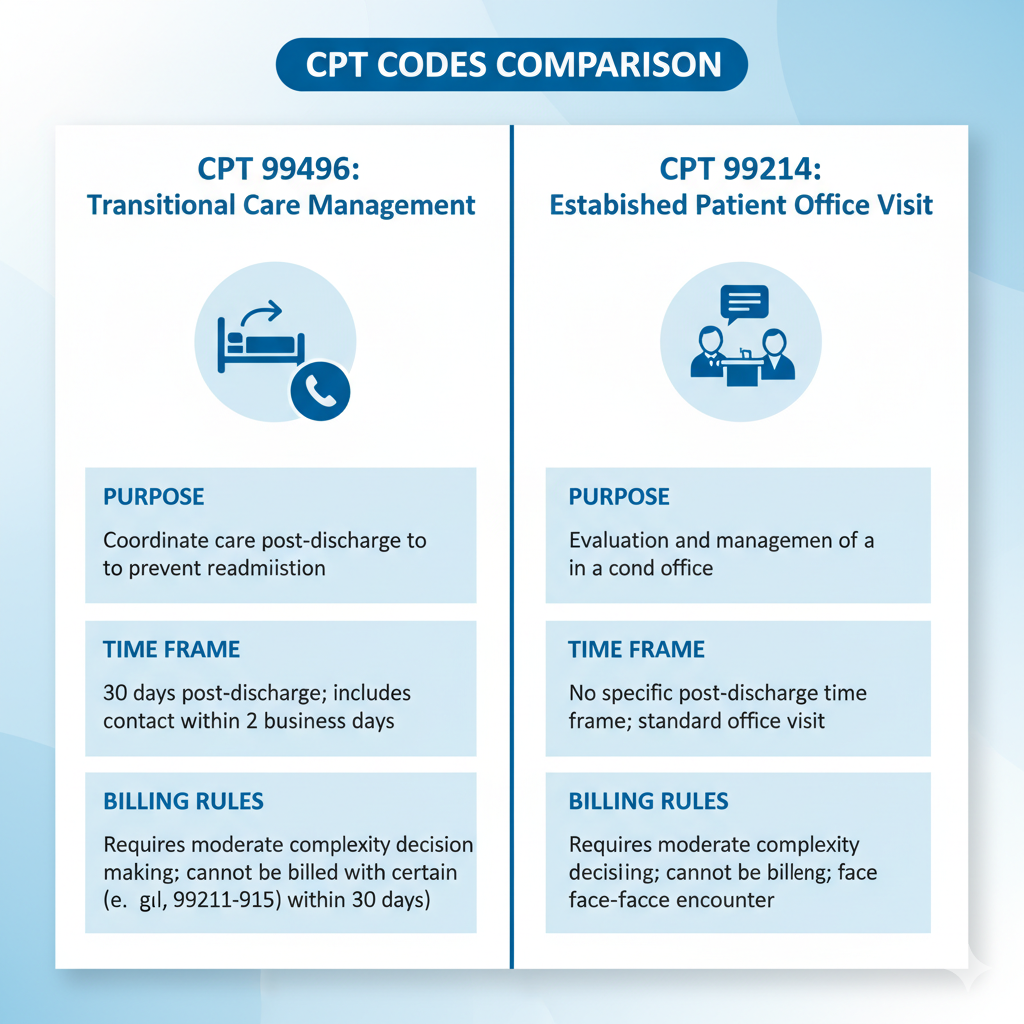
CPT 99496 is used for transitional care management (TCM) services provided to patients discharged from an inpatient hospital, partial hospital, or observation setting. It covers the period from the day of discharge through the next 30 days. To bill this code, providers must make contact with the patient within two business days of discharge and conduct a face-to-face visit within seven days.
The goal of CPT 99496 is to ensure continuity of care and reduce hospital readmissions. This service includes reviewing discharge information, coordinating follow-up appointments, managing medications, and addressing any complications or treatment changes. You can read the official definition in the CMS Transitional Care Management guide.
Understanding CPT 99214
CPT 99214 represents an established patient office or outpatient visit that involves moderate complexity in medical decision-making. It is typically used for follow-up visits, medication management, or condition monitoring. This code requires a detailed history, examination, and medical decision-making.
The AMA CPT guidelines specify that 99214 should reflect moderate complexity, making it a common code in outpatient settings where ongoing management of chronic conditions occurs.
Can CPT 99496 and 99214 Be Billed Together?
In most cases, CPT 99496 and 99214 cannot be billed together for the same patient within the same 30-day TCM period. The reason is that 99496 already includes the face-to-face evaluation and management (E/M) visit that occurs within seven days post-discharge. Adding 99214 for that same visit would result in double billing for services already covered under 99496.
However, you can bill 99214 separately if it is for a distinct and unrelated medical issue outside the TCM service period. For instance, if a patient is seen for an unrelated condition (such as diabetes management) after the TCM period ends, a 99214 may be appropriate. According to AAPC coding guidance, payers typically require clear documentation to prove the visit was separate and medically necessary.
Documentation Requirements
Accurate documentation is crucial when billing either code. For CPT 99496, your notes should reflect the discharge summary review, patient contact within two business days, medication reconciliation, care coordination, and a face-to-face visit within seven days.
For CPT 99214, the documentation must show detailed medical decision-making and ongoing management that is distinct from the TCM service. Each note should clearly state the purpose of the visit and why it was separate from transitional care. Providers can refer to the AAFP documentation standards for clarity on structuring notes for E/M visits.
Modifier Usage
If you find that both codes are legitimately billable, modifier 25 must be appended to CPT 99214 to indicate that it was a significant, separately identifiable E/M service performed on the same day as another service. This helps distinguish the additional office visit from the TCM visit.
The use of modifier 25 should be fully supported by documentation showing that the additional visit was medically necessary and unrelated to transitional care. You can review the proper application of modifier 25 in the CMS Evaluation and Management Services Guide.
Medicare and Payer Rules
Medicare and most private payers follow CMS guidelines, meaning CPT 99496 cannot be billed in conjunction with 99214 for the same patient during the 30-day TCM period. However, coverage policies can vary. It’s always important to verify payer-specific rules before submitting claims.
Providers should also remember that only one provider can bill TCM services during the 30-day period following discharge. If another provider attempts to bill 99214 during that same timeframe for a related issue, the claim may be denied. The CMS TCM Fact Sheet outlines these payer limitations in detail.
Example Scenario
Let’s consider an example. A patient is discharged from the hospital after a COPD exacerbation. The provider performs a follow-up call within two days and a face-to-face visit within seven days — these services fall under CPT 99496.
Two weeks later, the same patient visits the office for a hypertension checkup, which is unrelated to COPD management. Since this second visit is outside the TCM service window and for a different issue, the provider may bill CPT 99214 separately. Clear documentation should support the separation of these services.
Compliance Tips for Avoiding Denials
To avoid denials or audits:
-
Always confirm payer-specific guidelines before billing both codes.
-
Maintain clear documentation differentiating TCM from routine follow-up visits.
-
Use modifier 25 only when the E/M service is distinct and separately identifiable.
-
Ensure the medical necessity of each billed code is clearly evident.
Following these steps helps ensure compliance and minimizes audit risk. Detailed documentation guidance can be found in the AAFP E/M coding resources.