Preventive care visits are critical for maintaining long-term health, yet billing these services can be complex. CPT Code 99396 is a common preventive visit code that frequently faces denials if documentation or coding does not align with payer policies. Understanding its correct usage, documentation requirements, and reimbursement rules is essential for accurate billing and compliance.
This guide provides expert insights, practical examples, and industry best practices for coding and billing 99396 effectively.
What Is the 99396 CPT Code?
CPT 99396 represents a comprehensive preventive medicine evaluation and management service for an established patient aged 40–64. Unlike problem-focused visits, this code is used for preventive care that includes age-appropriate risk assessment, counseling, and anticipatory guidance.
This code is designed to help clinicians provide a thorough evaluation of overall health and to ensure preventive screenings and counseling are delivered consistently.
99396 CPT Code Description
The official description of 99396 is: “Periodic comprehensive preventive medicine reevaluation and management of an established patient; ages 40–64.”
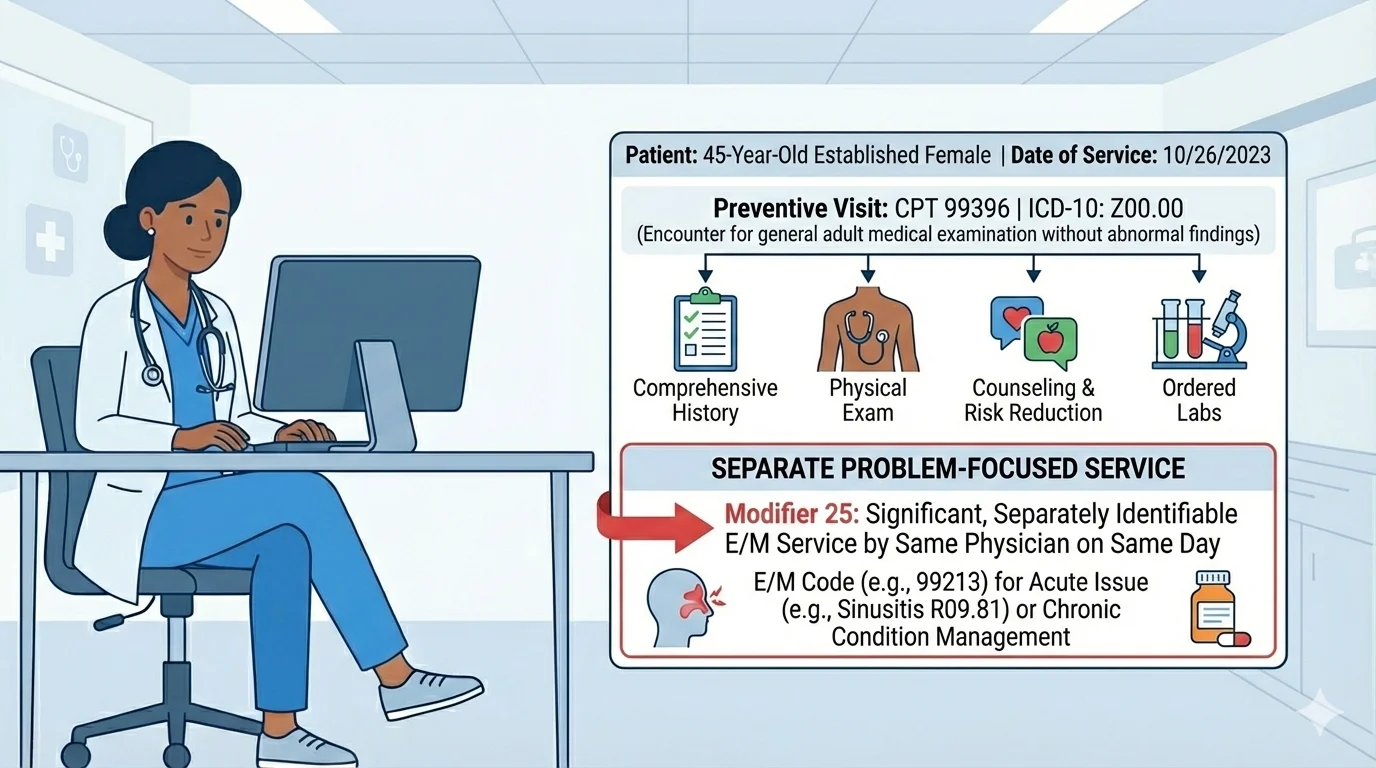
This service encompasses several critical elements: a detailed medical history, a complete physical examination, review of existing chronic conditions, preventive screenings, and counseling on lifestyle and health risks. It may also include immunization assessment and coordination of age-appropriate screenings.
The goal of the 99396 visit is not to treat acute illnesses but to maintain wellness, identify risks early, and guide patients in preventive care strategies.

Key Components of a 99396 Visit
Comprehensive Age-Specific History
A thorough patient history is the foundation of preventive care. Providers assess family medical history, past medical and surgical history, social factors, lifestyle behaviors, medications, and mental health screening. This history helps identify risk factors and guides the preventive plan.
Comprehensive Physical Examination
The physical exam should be complete and age-appropriate, covering all major systems including cardiovascular, respiratory, gastrointestinal, genitourinary, neurological, musculoskeletal, skin, and general appearance. Vitals and measurements should always be documented.
Counseling and Anticipatory Guidance
Preventive visits often include discussion of lifestyle and health behaviors. Counseling can focus on weight management, tobacco cessation, exercise, diet, and age-specific risk factors. Providers also advise on preventive screenings, immunizations, and health maintenance strategies.
Preventive Screenings
During a 99396 visit, clinicians may order screenings such as diabetes testing, lipid panels, mammograms, colon cancer screening, and other lab tests as indicated by the patient’s age and risk profile. These screenings support early detection and preventive care.
99396 CPT Code Billing Guidelines
Billing 99396 correctly requires attention to payer requirements and proper documentation.
A 99396 visit must remain preventive in nature. If a provider addresses a separate medical problem during the same visit, that problem-focused service should be billed separately using the appropriate office visit code, with modifier 25 appended. Documentation must clearly distinguish preventive services from problem-focused evaluation and management.
Insurance coverage varies. Most commercial plans allow one preventive visit per patient annually. Medicare does not cover 99396; instead, wellness visit codes are used for Medicare beneficiaries. Frequency limits should always be verified to avoid denials.
Documentation is critical. Notes should reflect a full history, comprehensive physical exam, counseling, preventive risk assessments, and any screenings or labs ordered. Additionally, 99396 is only valid for established patients; new patients require the corresponding new-patient preventive code.
99396 CPT Code Reimbursement
Reimbursement for 99396 varies depending on payer and region. Commercial plans generally provide higher reimbursement, while Medicaid rates may vary by state. Preventive visits are often covered at no cost to the patient when delivered in-network. Proper coding and documentation help ensure maximum reimbursement and reduce claim denials.
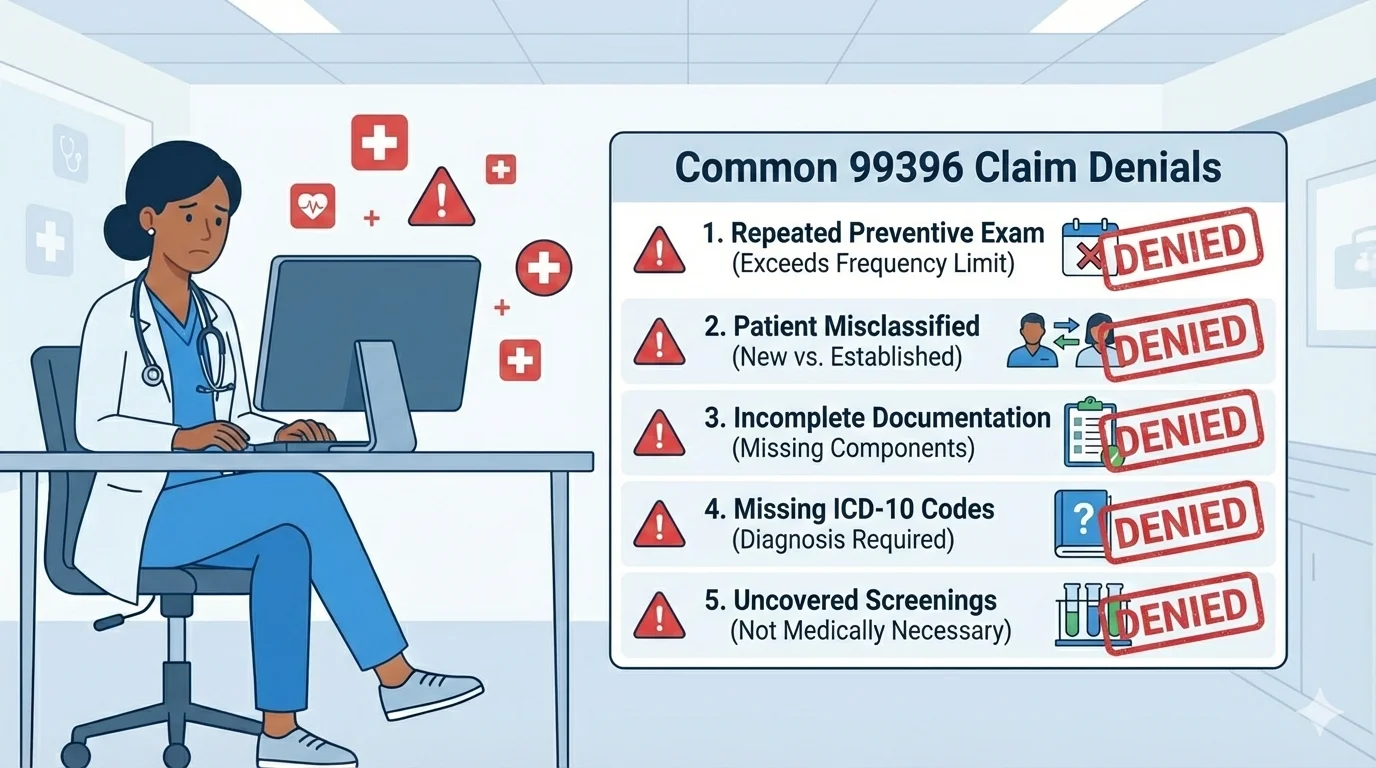
Common Reasons 99396 Claims Are Denied
Claims for 99396 are often denied due to the following issues:
-
The patient has already received a preventive exam within the allowable period.
-
The patient was incorrectly identified as established or new.
-
Documentation is incomplete or does not support a comprehensive preventive service.
-
Incorrect or missing ICD-10 codes.
-
Certain screenings are not covered under 99396 by the payer and require separate billing.
Correct ICD-10 Codes for 99396
Appropriate Z-codes support preventive care billing. Commonly used codes include:
-
Z00.00 – Routine general exam without abnormal findings
-
Z00.01 – Routine general exam with abnormal findings
-
Z13.220 – Lipid screening
-
Z13.1 – Diabetes screening
-
Z71.3 – Dietary counseling
-
Z71.82 – Exercise counseling
Using the correct codes ensures alignment with preventive care standards and supports payer compliance.
Billing Example
Consider a 45-year-old established patient arriving for an annual physical. The provider performs a comprehensive history, full physical exam, mental health screening, counseling, and orders labs for diabetes and cholesterol.
In this scenario, CPT 99396 with ICD-10 Z00.00 would be billed. If the patient also has a complaint requiring evaluation, such as knee pain, a separate office visit code with modifier 25 would be billed to capture the problem-focused service.