In the hierarchy of Evaluation and Management (E/M) codes, CPT code 99214 represents a significant level of clinical work. It is the "Level 4" office visit for an established patient, and billing it correctly is critical for the financial health of any practice. It signifies a visit that is a clear step above a routine follow-up, involving a "moderate" level of complexity or a substantial amount of provider time.
For RCM professionals and medical billers, 99214 is a high-value code that is also a high-priority target for payer audits. Since the 2021 E/M guidelines, the rules for justifying this code have completely changed. The focus has shifted away from counting historical elements and exam bullets to a more cognitive-based model: Medical Decision Making (MDM) or Total Time.
Understanding how to document and bill 99214 is not just best practice—it's essential for capturing earned revenue and preventing costly takebacks. This article provides a detailed breakdown of the 99214 billing guidelines, documentation examples, and common pitfalls.
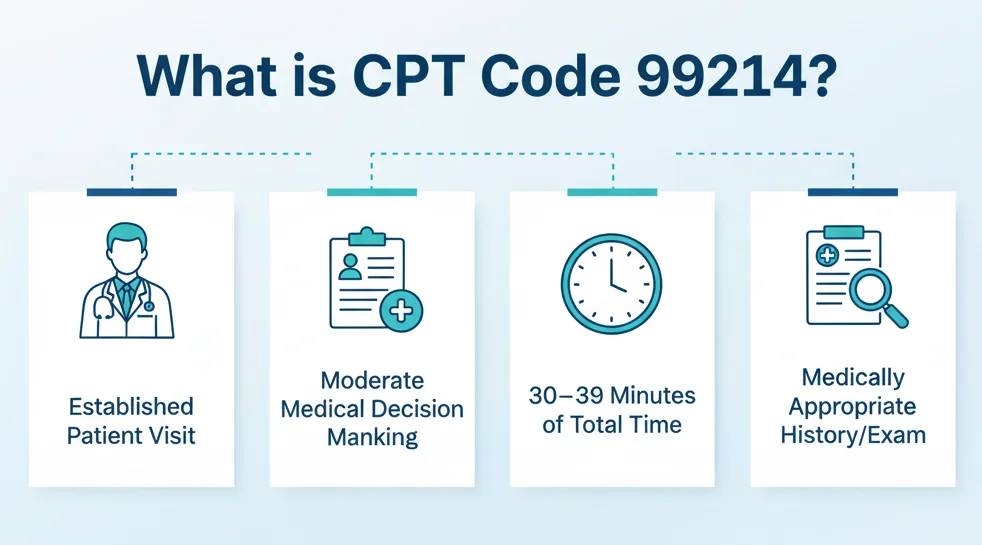
What is CPT Code 99214? The Official Definition
First, let's look at the official CPT definition. 99214 is used for an:
Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and a moderate level of medical decision making. When using time for code selection, 30-39 minutes of total time is spent on the date of the encounter.
Let's break down the key components:
-
Established Patient: This is non-negotiable. The patient must have been seen by the provider (or another provider of the same specialty in the same group) within the last three years. If the patient is new, you must use the 99204 code.
-
Medically Appropriate History and/or Examination: This is a major change from pre-2021. You no longer need to count 4 HPI elements or 10 ROS. The provider only needs to document the history and exam that is clinically relevant to the patient's complaint. The E/M level is not chosen based on the history or exam.
-
Moderate MDM or 30-39 Minutes: This is the core of the code. The visit must meet the criteria for either moderate-level MDM or total provider time.
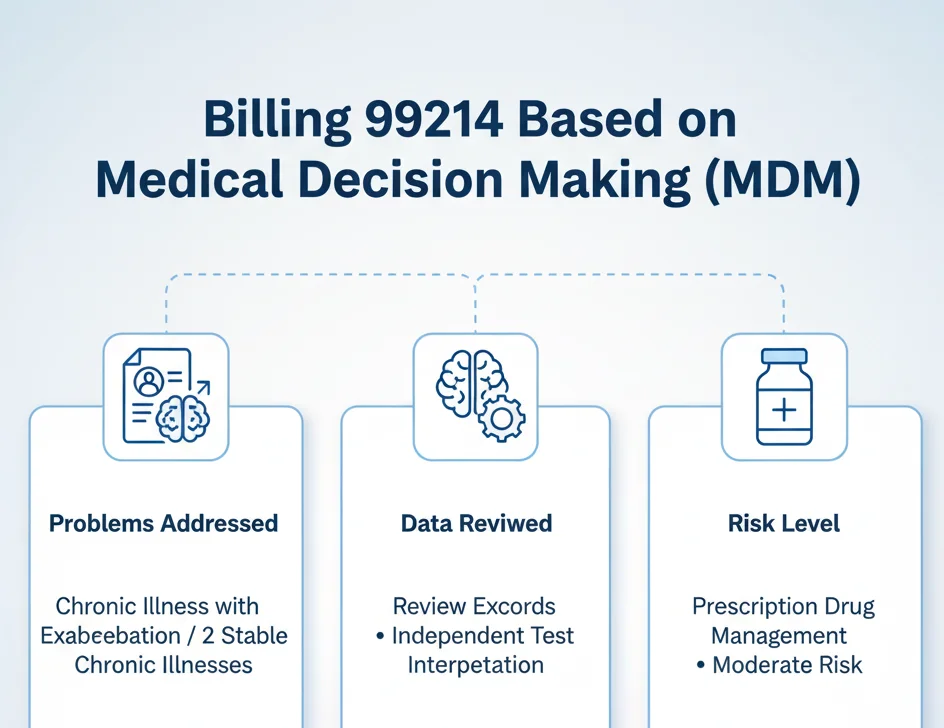
Pathway 1: Billing 99214 Based on Medical Decision Making (MDM)
This is the most common way to justify a 99214. The provider's documentation must meet the criteria for "Moderate" MDM. To qualify, the visit must meet or exceed the requirements for two of the three elements of MDM.
Here are the three elements and what "Moderate" means for each:
1. Number and Complexity of Problems Addressed
To meet the "Moderate" level for this element, the provider must document one of the following:
-
Two or more stable chronic illnesses. (e.g., A patient visit to manage both stable hypertension and stable type 2 diabetes.)
-
One chronic illness with exacerbation, progression, or side effects of treatment. (e.g., A patient with known asthma who is now wheezing and requires a new inhaler.)
-
One undiagnosed new problem with an uncertain prognosis. (e.g., A patient presenting with a new, undiagnosed breast lump.)
-
One acute illness with systemic symptoms. (e.g., A patient with fever, flank pain, and dysuria, indicating pyelonephritis.)
-
One acute complicated injury. (e.g., A patient with a head injury that did not involve loss of consciousness.)
2. Amount and/or Complexity of Data to be Reviewed and Analyzed
To meet the "Moderate" level for this element, the documentation must show one of the following:
-
Review of prior external records from a unique source (e.g., reviewing hospital discharge summary or notes from a specialist).
-
Independent interpretation of a test performed by another provider (e.g., provider personally reviews an EKG or X-ray image, not just the report).
-
Ordering of three or more unique tests (e.g., ordering a CBC, a BMP, and a chest X-ray all count as unique tests).
-
Discussion of management or test interpretation with an external provider or other qualified healthcare professional.
3. Risk of Complications and/or Morbidity or Mortality of Patient Management
This element is often the easiest to meet for a 99214. The "Moderate" risk category is met by one of the following:
-
Prescription drug management. This is the big one. If a provider starts a new prescription, modifies a current one (changes dose), or even just refills a medication they are actively managing, this meets the criteria. This is clearly defined by the American Academy of Family Physicians (AAFP).
-
Decision for minor surgery with identified patient or procedure risk factors.
-
Decision for elective major surgery without identified risk factors.
-
Diagnosis or treatment significantly limited by social determinants of health (e.g., a patient is unable to afford medication or follow-up care).
Pathway 2: Billing 99214 Based on Total Time
This pathway is more straightforward and objective. If the provider's work doesn't neatly fit the MDM criteria, but the visit was time-consuming, you can bill based on time.
For CPT code 99214, the requirement is 30-39 minutes of total provider time on the date of the encounter.
"Total time" is a critical definition. It includes all provider activities on the day of the visit, not just face-to-face time. This includes:
-
Reviewing charts, labs, or imaging before entering the exam room.
-
Performing the face-to-face (or telehealth) visit.
-
Documenting the visit in the EMR after the patient leaves.
-
Ordering medications, labs, or imaging.
-
Communicating with other providers or staff about the patient's care.
Crucial Documentation: If you bill based on time, the medical record must include a provider attestation statement.
-
Example Attestation: "I spent a total of 35 minutes on this patient's care on [Date of Service]. This time included reviewing recent specialist notes, conducting the visit, documenting my findings, and managing three prescription medications."
Without this statement, a time-based 99214 will be denied in an audit.
99214 Billing Examples: MDM in Action
Let's apply these rules to real-world scenarios to see the difference between a 99213 (Low MDM) and a 99214 (Moderate MDM).
Scenario 1: The Chronic Care Follow-Up A 60-year-old established patient presents for a follow-up of hypertension and hyperlipidemia.
-
Visit 1 (99213): The patient's BP is well-controlled on their current medication. Labs from last week are stable. The provider counsels on diet and continues all current medications without change.
-
MDM Analysis: This is "2 stable chronic illnesses." This could be Moderate for Problems, but the risk is Low (no prescription changes, just continuation). Data is "Limited" (review of labs). This visit is most appropriate as a 99213.
-
-
Visit 2 (99214): The patient's BP is elevated (150/92) despite compliance. Labs show high LDL. The provider discusses the findings and adds a new medication (e.g., a statin) and increases the dose of the patient's lisinopril.
-
MDM Analysis:
-
Problems: "One chronic illness with exacerbation" (uncontrolled hypertension) AND "one stable chronic illness" (hyperlipidemia). This meets Moderate Problems.
-
Risk: "Prescription drug management" (starting a new drug and modifying a dose). This meets Moderate Risk.
-
-
Result: Since 2 of 3 elements are "Moderate," this visit clearly qualifies as a 99214.
-
Scenario 2: The Acute Problem A 45-year-old established patient presents with a cough.
-
Visit 1 (99213): The patient has a cough and runny nose for 3 days. No fever. Lungs are clear. The provider diagnoses an acute, uncomplicated URI and recommends OTC fluids and rest.
-
MDM Analysis: "One acute, uncomplicated illness." This is Low Problems. Risk is Low (OTC management). This is a 99213.
-
-
Visit 2 (99214): The patient has a cough, fever of 101.5°F, and shortness of breath. Lungs show rales in the left lower lobe. Provider orders a chest X-ray and a CBC and starts the patient on an antibiotic for presumed pneumonia.
-
MDM Analysis:
-
Problems: "One acute illness with systemic symptoms" (pneumonia with fever). This meets Moderate Problems.
-
Data: "Ordering of two unique tests" (X-ray and CBC). This is "Limited," not Moderate.
-
Risk: "Prescription drug management" (starting an antibiotic). This meets Moderate Risk.
-
-
Result: Since 2 of 3 elements (Problems and Risk) are "Moderate," this is a 99214.
-
Reimbursement and RVUs for 99214
CPT code 99214 is reimbursed at a significantly higher rate than 99213, reflecting the increased work. Reimbursement is based on the CMS Physician Fee Schedule (PFS) and its formula of Relative Value Units (RVUs) multiplied by the national Conversion Factor (CF).
-
2024 National Average (Non-Facility):
-
Total RVUs: 3.85
-
2024 Conversion Factor: $32.7442
-
Average Reimbursement: 3.85 x $32.7442 = ~$126.06
-
This rate is a national average and will vary based on your geographic location (GPCI). Commercial payer contracts are often based on a percentage of this Medicare rate, so your specific reimbursement may be higher.
Common Billing Mistakes and Audit Risks
Payers heavily scrutinize 99214. Here are the most common errors to avoid.
1. Confusing 99214 vs. 99213
The biggest error is billing a 99214 for a 99213 service.
-
The Key Differentiator: The most common dividing line is prescription drug management.
-
99213 (Low Risk): A patient with stable hypertension whose prescription is simply refilled without provider management or changes.
-
99214 (Moderate Risk): A patient with hypertension whose medication is reviewed and purposefully continued as part of the management plan, or a patient whose dose is changed, or a new medication is prescribed. The documentation must show the provider managed the prescription, not just refilled it.
2. Misuse of Modifier 25
Payers are aggressively denying E/M services billed with Modifier 25 (Significant, Separately Identifiable E/M Service). This modifier is used when you bill a 99214 on the same day as a minor procedure (like a joint injection or skin tag removal).
-
Correct Use: A patient comes in for their 99214 visit to manage their diabetes and uncontrolled hypertension (a "Moderate" MDM service). During the visit, they also ask you to check their sore knee. You perform an exam and give them a joint injection (e.g., 20610). In this case, you can bill 99214-25 and 20610. The E/M service was separate from the pre-procedure work of the injection.
-
Incorrect Use: A patient comes in only for a scheduled knee injection. The provider briefly assesses the knee and performs the injection. This brief assessment is part of the procedure and is not a "significant, separately identifiable" E/M service. Billing a 99214-25 here is improper and a major audit risk. Your documentation must show two distinct services.
3. Billing Time without an Attestation
This is a simple but costly mistake. If your provider bills based on "30 minutes spent," but there is no signed attestation statement in the note, the service is non-compliant. The payer will downcode the service (likely to a 99213 or 99212), and you will have to pay back the difference.


